Scientific Program
Keynote Session:
Oral Session 1:
- Intensive Care Unit
Title: Italian Society of Anesthesia, Analgesia, Resuscitation, and Intensive Care expert consensus statement on the use of lung ultrasound in critically ill patients with coronavirus disease 2019 (ITACO).
Biography:
Dr. Luigi Vetrugno is an emergency consultant at the Department of Medicine, in the University of Udine, at the University-Hospital of Friuli Centrale, Udine, Italy.
Abstract:
Keywords: Consensus, Coronavirus disease 2019, Intensive care, Lung ultrasound.
Introduction:
The use of lung ultrasound (LUS) in the intensive care set- ting has increased during the coronavirus disease 2019 (COVID-19) pandemic. It is being employed as a diagnostic and monitoring tool in patients with COVID-19- related pneumonia a condition which in some cases evolves into acute respiratory distress syndrome (ARDS) [1]. Lung ultrasound presents many advantages over other imaging techniques: it is readily available at the bedside, thus avoiding the need to transport patients to the radiology department, and it is radiation-free and highly repeatable, making it suitable for lung monitoring purposes [2]. Lung damage in COVID-19 pneumonia is mainly localized to the peripheral regions of the lungs, thus easily accessible to ultrasound [3]. The sensitivity and negative predictive value of LUS for COVID-19 pneumonia are both higher compared with those for chest X-ray [4]. Moreover, many studies show a close correlation between LUS and computed tomography (CT) scan findings [5]. Given the prolonged need for mechanical ventilation in COVID-19 and long intensive care unit (ICU) stay, repeated lung assessments are usually required. CT remains the reference imaging technique or lung assessment, but it is unsuitable as a monitoring tool due to its use of ionizing radiation. It also necessitates patient contact with healthcare providers outside the ICU, increasing the opportunity for this highly infectious disease to spread. The quantitative evaluation of lung disease by means of the LUS score provides a reliable method for assessing lung aeration in both ARDS and COVID-19, and may further help in monitoring lung recovery and in the daily optimization of ventilation strategies (i.e., positive end- expiration pressure [PEEP] titration, and the use of prone positioning) [6]. Finally, LUS permits the early bedside detection of complications, such as pneumothorax [7] and ventilator-associated pneumonia [8]. As a consequence, LUS has earned a leading position in the management of COVID-19 patients, being a reliable, time-sparing, and easy-to-learn alternative to traditional imaging techniques [9, 10]. However, the recent literature is mainly focused on its applications within the Emergency Department [11]. Although Canadian Internal Medicine Ultrasound (CIMUS) experts recently established their recommendations for medical inpatients with COVID-19 [12], consensus guidelines dedicated to COVID-19 ICU patients and officially acknowledged by a national intensive care scientific society are lacking. To fill this gap, we aimed to produce an expert consensus on the bedside use of LUS in critically ill COVID-19 patients by a national panel of anaesthesiology and intensive care physicians.
Methods:
Consensus process design
This project was conducted according to a modified Del- phi method to reach consensus on key aspects of the use of LUS in critically ill patients with COVID-19. Discussions were based on the available scientific evidence as well as the panel of experts’ own clinical experience. The experts were selected by the project coordinators (LV and FM) based not only on their clinical and scientific interest in the topic [13] but also the opinion of intensivists who are not experts in LUS but who understand the context of critically ill COVID patients, and the potential role of lung ultrasound was invited. After an initial (online) kick-off meeting between the coordinators, the panellists, the methodologists (AC and DP), and the evidence review team (MI and DO), the project coordinators proposed a list of the most relevant clinical questions to the whole panel, which was then asked to submit a blind Boolean vote (“agree/disagree on the relevance”) as well as comments and proposals for their modification. In response, the coordinators made the appropriate changes to the clinical questions, which were finally approved by the whole panel through a second round of voting. The coordinators then assigned the work on each clinical question to a designated group of experts, each of which was led by a designated group head (PP, PN, EB, TB, and SM). The list of clinical questions and the final consensus-based statements.
Result:
The panel was composed of a total of 18 experts, 4 methodologists, and 2 senior heads. The panel produced a total of 20 statements. The criteria for a consensus of agreement (i.e., a score in the range 7 - 9 provided by 75% or more of respondents, and a median score value also within this range) were met for 18 out of 20 statements in the first round of voting. Consensus was not achieved in relation to statements no. 5 and no. 17 (see Fig. S 2, Additional file 2). After the second round of voting, consensus of agreement was achieved on all statements. The median score (plus interquartile range) and agreement percentage for all the statements contained in the final consensus report.
FIG 1: The lung ultrasound score (LUS) can be applied to assess the loss of aeration by dividing the thorax into 12 specific regions, six on the right and six on the left in supine or prone position assign each region a score from 0 (normal lung) to 3 (lung consolidation). Anterior, lateral, and posterior fields are identified by sternum, anterior, and posterior axillary lines. The entire examination can be performed without any change in patients position. Score: 0 = normal aeration (A-lines and lung sliding or maximum 2 well-spaced B-lines); score 1 = moderate loss of aeration (> = 3 well-spaced B-lines with lung sliding, coalescent B-lines/sub pleural consolidations occupying < 50% of the pleural line); score 2 = severe loss of aeration (> = 3 well-spaced B-lines with lung sliding, coalescent B-lines/sub pleural consolidations occupying clearly > 50% of the pleural line); score 3 = complete loss of aeration:lobar/hemi lobar consolidation with predominant tissue like pattern which will lead the patient into critical condition. 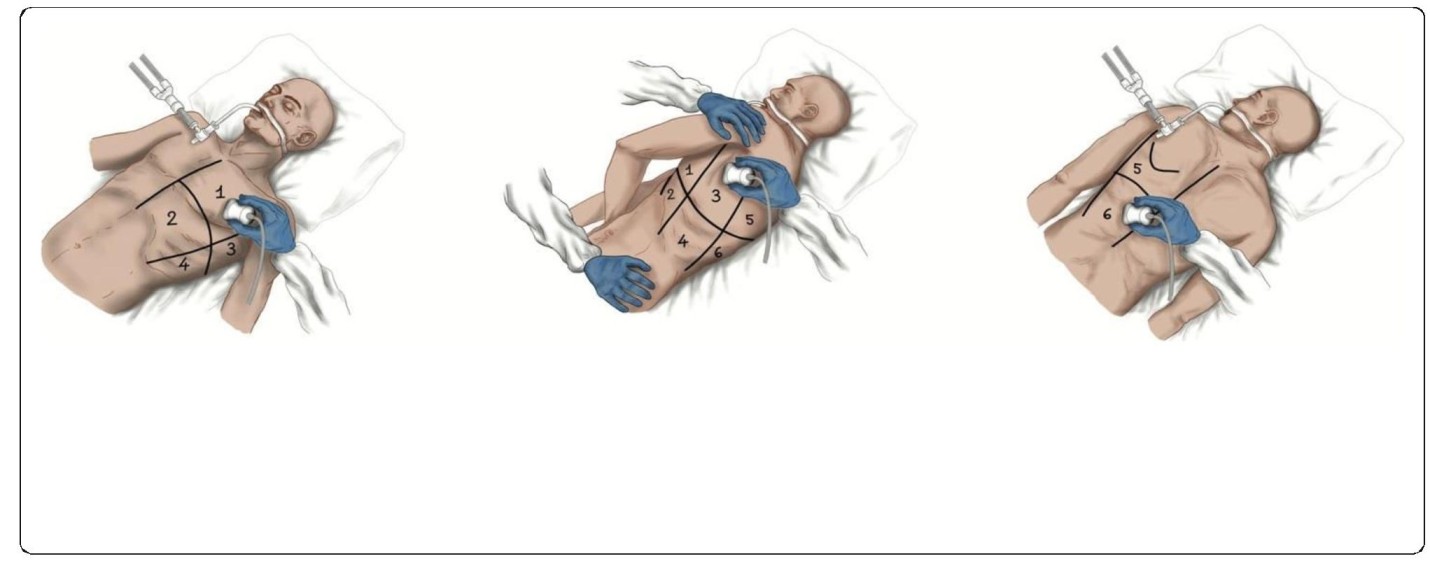
Conclusion:
The Lung Ultrasound Working Group of the Italian Society of Analgesia, Anaesthesia, Resuscitation, and Intensive Care produced 20 consensus statements on the use of lung ultrasound in COVID-19 patients admitted to the ICU. This expert consensus strongly suggests integrating lung ultrasound findings in the clinical management of critically ill COVID-19 patients.

Dr. Veena Mohan
Head of the Accident and Emergency Department, Gutersloh District Hospital, Germany.Title: COVID 19 Pandemics Mental Impact on the frontline nurses in the emergency department.
Biography:
Abstract:
The largest pandemic , the world has seen since 2020 March- COVID-19, has been the culprit for many pitfalls, new rules and regulations, economic problems and most importantly responsible for the mental declination of the healthcare workers, specially the nurses.
In this dissertation, I have analysed 29 studies from China, Singapore, Iran, Spain, India, Pakistan, Bangladesh and America regarding the impact of the COVID pandemic on the psychological condition of the nurses. It was transparent through the studies that the nurses suffered greatly under depression, anxiety, stress, PTSD and insomnia due to the uncertain and highly stressful situation caused by the pandemic. The dissertation and analysis of the study was specified for the frontline nurses as they faced instability and stress mostly during the pandemic. This analysis sheds light on the fact that we have to react to this problem and generate ways to help the nursing force to cope with this negative mental declination during the pandemic, so that the world doesn’t face an extinction of the nursing force. This support to the nurses will also help the nursing profession to project attractively on the coming generation.
Title: Paramedic assignment in field hospital
Biography:
Edward Vershilovsky served as a paramedic for 15 years in the Israeli national emergency medical service. During his service he worked with the International Red Cross during the 2014 crisis in Ukraine, took part of the Israeli delegation to Panama, field hospital missions in Nepal and Equatorial Guinea. Edward served as chief instructor in Israeli national EMS paramedic training center. Nowadays, Edward is a clinical director for PerSys Medical, a manufacturer of medical devices intended for emergency interventions.
Degrees held: B.EMS (bachelor of emergency medicine), MPH (Master’s mergency and disaster management). Flight paramedic
Abstract:
Paramedics (EMT-P) are leading members of emergency medical teams around the world. In Israel, paramedics are team leaders of civilian EMS teams, senior caregivers on a battalion level in IDF and they carry the medical responsibility in military and civilian rescue units. Israeli EMT-P holds permissions to manage advanced airway (intubation, supraglottic AW,surgical AW), perform needle and chest thoracostomy, insert a gastric tube and Foley catheter , insert a central line and provide sedative agents. The training of IDF paramedics is similar to the civil training with similar permissions.
During IDF field hospital mission in Nepal in 2015, 5 IDF paramedics joined the hospital team and were stationed in different hospital wards: ER, OR, ICU, admission ward – a shift from their primary role at the rescue mission.
The second opportunity to utilize paramedics in hospital setting was during IDF medical assistance mission in Equatorial Gunea. Paramedics were stationed in the ER,OR and field clinics.
During the presentation, I discuss the challenges, opportunities, success, failures and lessons learned from paramedic functioning in a hospital setting.

Dr Tom Jose
Associate specialist at the Urgent Care Centre, Royal Preston Teaching Hospital, United Kingdom.Title: Haemolytic anaemia caused by Epstein-Barr virus infection in an adult, picked up in an urgent care setting.
Biography:
Dr Tom Jose has pursed his MBBS from Mahatma Gandhi University, India MRCEM in 2014, EBEEM in 2018 from Belgium, and currently working as associate specialist in A&E Royal Preston Teaching hospital, UK from 2018- till date.
Abstract:
Introduction:
Infectious mononucleosis caused by Epstein-Barr virus is common in children characterised by fever, malaise, sore throat and lymphadenopathy. Autoimmune haemolytic anaemia is a rare complication of EBV infection occurring only in 1-3% of patients1. Haemolysis should be considered in all patients with infectious mononucleosis who develop jaundice to avoid diagnostic delay and a deleterious outcome.
Aims and objectives:
We present an interesting case with autoimmune haemolytic anaemia as a complication of EBV infection, to increase its awareness and early diagnosis and treatment.
Key words:
Anaemia, jaundice, haemolysis, autoimmune, haemoglobin
Case report:
In this article, we present a 22-year-old previously fit and well gentle man, sent from army barracks to rule out jaundice as his colleagues noticed mild yellowish tinge to the face. He didn’t have any other symptoms. Examination revealed mild jaundice and pallor. There was no lymphadenopathy or hepatosplenomegaly. Laboratory investigations in the UCC showed a Hb of 65, and deranged liver functions. Inpatient investigations revealed reticulocytosis, raised LDH, and EBV serology consistent with recent Acute Epstein-Barr virus infection. It was concluded that he was having Coombs negative autoimmune haemolytic anaemia as a complication of EBV infection. His counts recovered spontaneously while in the hospital with negative parameters for haemolysis without starting any immunosuppressive therapy.
Discussion:
Infectious mononucleosis is caused by Epstein – Barr virus infection characterised by fever, sore throat, lymphadenopathy and atypical lymphocytes. EBV is considered an infrequent cause of autoimmune haemolytic anaemia (AIHA)2. AIHA is caused by formation of IgM antibodies against the polysaccharide antigens of red blood cells, causing agglutination in low temperatures leading to complement activation and haemolysis5. Treatment consists of IV immunoglobulin and oral steroids4. In this particular case, blood counts improved spontaneously without needing immunosuppressive therapy.
Conclusion:
Autoimmune haemolytic anaemia should be considered in infectious mononucleosis patients presenting with anaemia, though it is a very rare complication8. Treatment with IV immunoglobulin and oral corticosteroid appear to be beneficial in these cases10.
Acknowledgements:
The authors would like to thank Mr Yogdutt Sharma, Medical director of GTD for his assistance with proof-reading and editing the article.
Conflicts of interest:
There are no conflicts of interest.
Author’s contributions:
All authors have critically reviewed and approved the final draft and are responsible for the content of the article.
Oral Session 2:
- Medical Toxicology

Dr Nancy Saral Mary
MEM II yr Resident, Department of Emergency Medicine, George Washington University.Title: HAIR DYE POISONING:
Biography:
Abstract:
An estimated 1 million people worldwide die by suicide every year. According to W.H.O, 381 suicide cases are reported daily in India. In India most of the suicide is committed by poison mainly pesticide. Nowadays Hair dye poisoning is also emerging mainly among the female. Age group of 15 to 45yrs. One of the widely chosen means of suicide is Poisoning in south India mainly among middle class people in our country. Trend of Consuming hair dyes for suicide has increased. It is less costly and widely available.
Case Study:
A 20 -year-old female presented to ED with Alleged H/o intentional consumption of hair dye poisoning (content of para phenylene diamine, propylene glycol, resorcinol, sodium lauryl sulphate liquid, light liquid paraffin, herbal extracts along with preservatives and perfumes) about 100 ml at her residence around 12p.m. She had facial swelling with edema of lips, swelling of neck and tongue; stridor was present and difficulty in speaking.
Report:
No H/o Altered sensorium/ Seizure/ Decreased urine output/ Dark color urine/ vomiting/ Blurring vision. On receiving BP: 110/80 mmHg PR: 100/min Temp: 98.2°F, Spo2: 98 % with oxygen by mask, CBG: 146mg/dl, GCS: E4 M6 V4 14/15.
General Examination:
Patient was conscious, oriented and afebrile, on exposure facial swelling with edema of lips, swollen neck and tongue. No external injury.
Systemic Examination:
CVS: S1S2 (+), No added sounds RS: B/L AE (+), No added sounds CNS: B/L PERL, NFND, P/A: Soft, mild epigastric tenderness with no organomegaly P/R: Normal, P/V: Normal.
Comorbities: Nil; Previous Medical/Surgical History: NIL
Investigations:
ABG, Beta-HCG, CBG, ECG, USG, Complete metabolic panel, Sr. Calcium, CPK Total, urine.
Myoglobin, LFT, RFT, Peripheral smears, Chest X-ray was ordered.
Airway & Breathing : In order to protect the airway, patient was intubated and put her on mechanical ventilator.
Circulation: IV line is secured, and hypotension is corrected by IV fluid bolus.
Decontamination: Gastric lavage was done to the patient with activated charcoal
Laryngeal edema and ARDS: she was treated with injection hydrocortisone 200 mg stat and Neb. Adrenaline inhalation and antihistamines for angioneurotic edema.
Enhanced Elimination: Forced Diuresis by giving isotonic saline + sodium bicarbonate+ Lasix.
Initial ABG SHOWED SEVERE METABOLIC ACIDOSIS for which she was treated with Inj. Sodium
Bicarbonate stat dose followed by sodium bicarbonate infusion pump.
Dispatch:
Patient was shifted to ICU.
On the 2nd day, the patient developed dark coloured urine with a decreased urine output and pedal edema.
Laboratory investigations revealed:
Blood urea of 180 mg/dl (7 – 30 mg/dl) | Serum creatinine of 5.6 mg/dl (0.7 – 1.2 mg/dl) | Serum creatinine phosphokinase (CPK)1750 U/L(Male: 39 – 308U/L & Female: 26- 192U/L).
Urine Myoglobin was positive.The liver function tests were normal and the peripheral smear did not revea evidence of hemolysis
Ultrasonography of the abdomen showed normal size and echo texture of both kidneys.The chest x-ray and electrocardiogram were also normal.
Patient was treated with Inj. Hydrocortisone and anti-histamine in view of stridor and respiratory distress which resolved after 2 days of treatment.
On the 3rd day, she developed rhabdomyolysis and ARF. Her Blood urea and creatinine levels were elevated and ABG shows severe metabolic acidosis. She was managed initially with forced alkaline diuresis and in view of severe metabolic acidosis and hyperkalaemia she received 3 sittings of haemodialysis. Acute renal failure resolved over 6 days with dialysis.
She was clinically improved and extubated and put on NIV to prevent further atelectasis of both lungs and transferred on High Flow Mask and graded clinically and discharged home on 9th day of admission after obtaining counselling.
PARAPHENYLENE DIAMINE (PPD) (C6H4(NH2)2:
Main component aromatic amine not found in nature a toxic substance since 1924.PPD is banned in certain countries like Germany, France, Sweden, Sudan, etc. Derivative of para nitro Aniline (coal-tar derivative).White in colour which turns brown when exposed to air. On Oxidation it produces- Bandrowski’s base – Anaphylactic, Mutagenic and Toxic Properties. Severity of the poisoning is directly proportional to the Concentration of PPD.
PPD – Severe Angioneurotic Edema, Rhabdomyolysis and Intravascular Hemolysis.
Lethal Dose:
Severity of the poisoning Increases with the Dose (7 to 10 gms), 3gms sufficient to cause systemic complication
Resorcinol:
Phenolic Derivative, Corrosive | Seizure, Lethargy, Coma, Death
Nausea, Dyspnea, Hypotension, Diaphoresis, Salivation, Methemoglobinemia, Pulmonary edema
Propyelene Glycol:
Metabolic Acidosis, CNS depression, Arrhythmia, Renal dysfunction
EDTA Ethylene diamine tetra acetic acid Sodium - Hypocalcaemia ( due to rhabdomyolysis) NEPHROTOXIC COCTAIL
PPD + Resorcinol + Propylene Glycol.
Pathophysiology:
Para phenylene diamine: Severe Angioneurotic Edema, Rhabdomyolysis and Intravascular Hemolysis.
Rhabdomyolysis:
Leakage of calcium ions from Smooth ER, followed by continuous contraction and irreversible change in muscle structure. Rhabdomyolysis along with Hypervolemia and PPD metabolites causes Acute Renal Failure.
Propylene glycol:
Hyperosmolarity, increased anion gap, metabolic acidosis, CNS depression, Arrhythmia and Renal dysfunction.
Resorcinol:
Eye, skin, oral and gastrointestinal injuries, renal toxicity.
Phase 1:
Vomiting | Gastritis | Hypertension| Vertigo| Severe Edema of Face, Neck, Tongue, Pharynx and Larynx with Respiratory Distress –Stridor | Convulsions
Phase 2:
Hemolysis | Rhabdomyolysis: Chocolate brown colour of the urine | ARF | Hypocalcaemia
Phase 3:
Muscular Edema | Multi organ Failure | Shock
Stages of Angioedema:
Cricopharyngeal edema + Laryngeal edema Asphyxia Respiratory distress and Hypoxia Respiratory failure
Cause of death:
Respiratory Obstruction | Renal Failure | Arrhythmia | ARDS
ECG shows non-specific changes with frequent premature ventricular complex suggesting myocarditis after hair dye ingestion.
ECG shows ventricular tachycardia suggesting myocarditis after hair dye ingestion.
Diagnosis:
History of consumption or materials got from the scene | Clinical Features | RFT | CPK | Serum Calcium | Urine dip stick | Thin layer chromatography
PPD can be diagnosed by thin layer chromatography on silica gel ( solvent system benzene, ethyl acetate or hexane acetate) and sprayed with 0.2% solution of potassium dichromate as chromogenic reagent to give a pinkish brown spot.
Myoglobinuria: urine dip stick or urine color change
Treatment:
No specific Antidote | Treat the complications | Gastric Lavage is useful within 1 hour of presentation | Activated Charcoal (1g/kg) | Mainly Symptomatic and Supportive | Emergency – Airway protection : Intubation or Tracheostomy
Conclusion:
In Pediatric also accidental ingestion of Hair dye poisoning the management is the same. Mortality depends on the amount of hair dye ingested, the time interval between consumption and intervention, hyperkalaemia, hypocalcaemia, and hypophosphatemia; and mortality rates varied between 0.03% and 60%. Whenever Stridor due to upper airway oedema, Rhabdomyolysis, Haemoglobinuria.
Myoglobinuria, ARF develops in a poisoning Hair dye poisoning should be considered. Early Diagnosis & Intervention will save a life. In addition, Community awareness & Health education. Remembering the fact that there is no specific antidote for PPD, the patient must be managed by watching like a hawk. In conclusion, hair dye poisoning is a life-threatening emergency which requires life-saving emergency resuscitation and early management of anaphylaxis. Early recognition of rhabdomyolysis, early prevention of acidosis and early initiation of forced alkaline diuresis prevent ARF minimizing the need for dialysis.
We are uncertain of the time of development of Renal Failure following ingestion of PPD and hence all patients should be monitored in the hospital for development of renal and other complications.Hair Dye Poisoning: Kills the kidney, hits the heart, cuffs the trachea.

DR SUJAY.S
Sri Atal Bihari Vajpayee Medical College & Research Institute, Bowring & Lady Curzon Hospital., IndiaTitle: Multiple Infarcts in Brain Following Viper Snake Bite
Biography:
Dr Sujay S completed his M.B.B.S from Madras medical college in 2017 and completed his MD in emergency medicine from “Kempegowda Institute of Medical Sciences”,in 2021.
He is currently working as a senior resident at “Sri Atal Bihari Vajpayee Medical College and Research Institute”, Bowring & Lady Curzon Hospital, Bangalore.
He also works as an International instructor for AHA BLS and ACLS courses.
Abstract:
INTRODUCTION:
Multiple infarcts following viper snake bite is a rare complication but fatal. Venom exhibits anti-coagulant and procoagulant effects. Haemorrhagins present in viper venom are complement mediated toxic components that may result in vascular spasm, endothelial damage and increased vascular permeability which lead to toxic vasculitis resulting in thrombosis which results in cerebral infarction.
CASE HISTORY:
A 50 year old male presented to ED with alleged history of snake bite 2 days back and had taken ayurvedic medication. Patient was in altered sensorium, irritable and restless.
Vitals were Pulse: 100bpm; BP: 90/60mmhg; GCS: E1V2M2.
Patient was intubated in view of low GCS. RFT, LFT, Coagulation profile was normal but WBCT was >20mins. CT brain was showing multifocal infarcts in bilateral frontal, parietal, Left temporo occipital cortex, left thalamus. Patient received 30 vials of ASV. His condition continued to deteriorate and patient died 3 days post admission.
CONCLUSION:
In summary snake bite are common particularly in rural areas and there is a need to keep the possibility of cerebral infarction as one of the complications.



