Scientific Program
Keynote Session:
Oral Session 1:
- Brain Tumors & Neurosurgery

Ahmad Fawad Pirzad M.D
Neurosurgery department of Aliabad Hospital, Kabul University of Medical Sciences (KUMS).Title: Brain Hydatid Cyst cases in Neurosurgery ward of Aliabad Hospital
Biography:
Ahmad Fawad Pirzad M.D is working as the Chief of Neurosurgery dept. (KUMS), Afganisthan. He is aslo the President of Afghanistan Neurosurgical Society and he also published a book by name Pirzad’s Textbook of Neurosurgery. His research interests are Dowling-Orlando technique, Echinococcus, Brain Hydatid Cyst
Abstract:
Introduction: Brain Hydatid Cyst is one of rare causes of Intracranial Space Occupying Lesion (ICSOL), Hydatid disease is caused by the infestation of the larvae of Echinococcus. The definite hosts of Echinococcus are various carnivores, the common being the dog.. Humans get infected through the feco-oral route by ingestion of food contaminated by dog feces containing ova of the parasite or by direct contact with dogs. Brain involvement with Hydatid disease occurs in 1-2% of all Echinococcus granulosus infections.
Objective: Isolated cerebral Hydatid disease is a rare manifestation of it and discuss their mode of presentation, radiological features, operative procedure and outcome. The literature concerning isolated cerebral Hydatid disease is reviewed.
Method and material: Case series study, patient files.
Result: There were report 9 cases of successfully operated of Brain Hydatid Cyst from 2014 -2018.
In this report, we analyze nine cases of isolated cerebral Hydatid cysts In our two cases, radiological features and surgical approaches were different .
Patient chief complain was: Headache 77%, Vomiting 35%, Convulsion 45%, Vision problem 30%, Motor deficit 50%, Dysphasia19%, Sensory disturbances33%.
Cyst localization: left side of Brain 63%, right side of Brain 37%
Sex: 8 female and 1 male
Operation: by local Anesthesia. Craniotomy and Dowling-Orlando technique 7 cysts completely removed and 2 cases ruptured, and reported later.
Anthelmintic medicine before and after operation continued by consultation of Internist.
Conclusion: Brain involvement with Hydatid disease occurs in 1-2% of all Echinococcosis Granolosis infections. Isolated cerebral Hydatid disease is a rare manifestation of it. In this report, we analyze nine cases of isolated cerebral Hydatid cysts and discuss their mode of presentation, radiological features, operative procedure and outcome. In our two cases, radiological features and surgical approaches were different from one another. The literature concerning isolated cerebral Hydatid disease is reviewed.
Oral Session 2:
- Central Nervous System
Title: Foramen Magnum Meningioma: A case report and review of literature
Biography:
Prarthana Subedi is a 4th year medical student at the Nepalese army institute of health sciences college of medicine, Nepal and she is also a member of President : Walter E. Dandy Neurosurgical student club of Nepal.
Abstract:
Introduction:
Foramen magnum meningioma’s are rare forms of meningioma’s. Among all the meningioma’s, only about 1 to 3% arises at foramen magnum level. 1The neurological signs and symptoms are very bizarre for these meningioma’s. There are very few case reports on Foramen Magnum Meningioma’s in Nepal
Case presentation:
A 62 year old male with co-morbidities like, Right sided hemiparesis, Hypertension and Diabetes Mellitus II presented to the Emergency department or an increase in weakness of the right arm and leg for 2 days and Fever for 1 day. He suffered a stroke 2 years ago with right sided hemiparesis. CT images revealed a mass in the poster lateral foramen magnum area. Meningioma of Foramen magnum was suspected, which was confirmed by MRI. The tumor was excised by far lateral approach with laminectomy at the level of C1 and C2 vertebrae, the operation lasting for 8 hours2 anticipated complications were blood loss, infections and CSF leak post-surgery.
Follow up outcomes could not be ascertained because of the COVID lockdown.
Conclusion:
Foramen magnum meningioma’s are rare tumors arising from the Craniocervical junction with indolent presentation and a late diagnosis. If left untreated, the outcomes can be debilitating, with respiratory arrest. We present a case of a 65 year old male presented to our department treated with the resection of the tumor with a far-lateral approach. The follow-up outcomes of the patient however cannot be ascertained. This is one of the few case reports on Foramen Magnum Meningioma coming out of Nepal.
References
- Bureau M, George B. Classification system of foramen magnum meningiomas.J Craniovertebr Junction Spine. 2010 Jan; 1(1):10. [ DOI | PubMed | Full Text ]
- Borba LA, de Oliveira JG, Giudicissi-Filho M, Colli BO. Surgical management of foramen magnum meningioma’s. Neurosurgical review. 2009 Jan; 32(1):49-60. [DOI | PubMed ]
Oral Session 3:
- Neurosurgery
Title: Epistaxis as first clinical presentation in prolactinoma
Biography:
Currently in the 5th year of residency in the department of neurosurgery at Military Hospital of Instruction of Tunis,TUNISIA.
Kaouther Somrani is working as a resident on neurosurgery in the neurosurgery department at the Military Hospital of Instruction of Tunis, Tunasia.
Abstract:
Introduction:
Prolactinoma is the most frequent type of pituitary tumor. It may be particularly giant and invasive. It has wide way of presentation. Epistaxis due to prolactinoma has been rarely reported in the literature.
Material and methods:
We report the case of a 48 year old man presented with epistaxis and headache since two months, who was admitted for an acute worsening of his headache and epistaxis without visual troubles. Otherwise he had erectile dysfunction for 2 years.
Results:
The patient was fully conscious and didn’t present any localization sign. The examination of the cranial nerves was normal. He had gynecomastia and morbid obesity. Brain MRI revealed a pituitary macroadenoma which eroded the sella turcica with stigmata of recent bleeding. Hormonal tests concluded to a prolactinoma. The patient received cabergoline with favorable clinical course.
Discussion and conclusion:
Pituitary adenoma presents with headache, visual deterioration and various kinds of endocrinopathies. Rarely pituitary adenoma especially prolactinoma can present with epistaxis.
The first line treatment is based on dopamine agonist which can lead to a reduction of the tumor volume and disappearance of epistaxis.
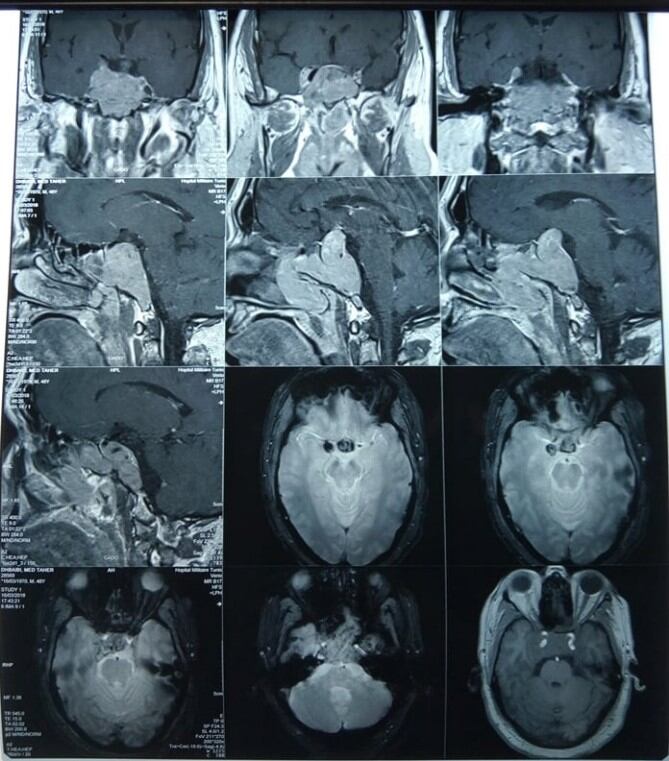
Figure 1: Brain MRI in coronal and sagittal view, in gadolinium-enhanced T1 weighted showing the pituitary macroadenoma with erosion of the sella turcica with stigmata of recent bleeding.
Recent Publications
1.Godey B, Morandi X, Le Gall F, Feat S, Brassier G, Le Clech G (1999) Pituitary adenomas with infra-sellar extension into the nasopharynx.J Laryngol Otol.1999; 113:1109-11.
2.Kleinschmidt-Demasters BK, Lillehei KO (1998). Pathological correlates of pituitary adenomas presenting with apoplexy.Hum Pathol.1998;29:1255-65
3-P Kumar Chaurasia (2011) Epistaxis as first clinical presentation in a child with giant prolactinoma: Case report and review of the literature J Pediatr Neuroscience.2011 Jul;6(2):134-7.
4- Sahoo JP, Kamalanathan S, Parida PK, Pillai V. (2015)A giant prolactinoma with nasopharyngeal extension presenting with nasal blockage and epistaxis.BMJ Case Rep. 2015 Apr 29;2015:bcr2014208811
5. Iglesias P, Diez JJ (2016) Macroprolactinoma: a diagnostic and therapeutic update.QJM. 2013 Jun;106(6):495-504
Oral Session 4:
- Neurology
Title: NEWS ON NEUROPALARIA: BROCA's aphasia complicating encephalitis acute malaria, Approach Neuroadapted Therapeutics: Place of Citicholine and Neuroregulators in prevention, reduction of sequelae neurological and morbidity and mortality.
Biography:
Lamirez Diasivi Nzuzi is working for the department of neurosurgery at Mont-Amba University Hospital Center (CHMA), University of Kinshasa.
Abstract:
Cerebral malaria, acute malarial encephalitis due to Plasmodium falciparum: is an acute brain injury whose outcome may be fatal can lead to polymorphic neurological sequelae: hemiplegia / hemiparesis, speech disorders (motor aphasia de Broca, Sensory aphasia of Wernicke), behavioral disturbances, cognitive impairment, blindness, secondary epilepsy. In Africa Sub-Saharan, and more particularly in the DRC, Neuropalaria, knows a high frequency of neurological lesions with a very high lethality and the seriousness of their repercussions on the fate of the children who are victims of it. The neuropathological severity of acute malarial cerebral aggression is correlated with the high parasite density, with the phenomena of sequestration and cytoadherence, the inflammatory process, the presence of the factors of bad prognosis or ACSOS, the diagnostic and therapeutic delay; and the antimalarials, do not modify the evolutionary process of neurological lesions and those of sequelae. An approach Neuroadapted therapy (Citicholine and neuroregulators) introduced in our patients, from the acute phase (from D0: in first 24 hours / first 6 hours +++ to 7 days), until the stabilization phase (D0- 30 days), allowed us to: Improve perfusion of the areas of ischemic brain suffering, regulation of cerebral metabolism (aerobic glycolysis +++) and reduction of cerebral edema (vasogenic, cytotoxic +++); delay the evolution of the destruction of the neuronal membrane and neuronal degeneration; limit and block ischemic cascades leading to neuronal necrosis; Improve the prognosis and dramatic rapid recovery, speech recovery and significant reduction in other neurological sequelae, but also death-mortality.
To date, acute malarial encephalitis should be considered in mind as a normotensive ischemic stroke. post-infectious, until proven guilty, in the light of the neuroanatomo-clinical correlation, of the neurophysio- pathologies induced in acute and secondary cerebral aggression.
Goal:
Management of acute malarial encephalitis and its acute complications, and to propose a Neuroadapted therapeutic approach, by demonstrating the action of Citicholine and neuroregulators on Broca's area.
Methodology:
A serial study of cases admitted to the Emergency and Neuropediatrics Department for acute malarial encephalitis complicated by aphasia de Broca and other neurological sequelae.
Results
In the absence of certain medical files available and in the insufficiency of clinical and para-clinical data found in certain records, of the 30 patients registered for acute malarial encephalitis complicated by neurological deficits during the period of March 2021, we describe that two cases of Broca's Aphasia on Acute Malarial Encephalitis in two patients born and residing in DRC, Kinshasa. The first case; a 9-year-old male child admitted to the neuropediatric emergency room for tonic-clonic seizures and headaches, in his antecedents, no notion of previous seizure episode, no convulsors and epileptics in the family. Treatment received elsewhere, Quinine, Ciprofloxacin and Diazepam; In whom we note mainly at physical examination, Heart rate at 140 bpm, Respiratory rate at 40 cpm, Temperature at 38 ° C, Coma with convulsions
Tonic-clinical, febrile on palpation, colored eyelid conjunctivae and anicteric bulbar conjunctiva, an abdomen not bloated, sensitive to medium ureteral points and without organomegaly, Deep coma, Soft neck and no signs of neuro-irritations meningeal, isocoric and reflective pupils. On paraclinical examination, Hb at 12 g / l, occasional glycemia at 109 mg / dl, GE: Tropho +++, GB: 16000 elt and FL: N60% L40%; Widal (TH: 1/160, TO: 1/160), Blood ionogram, CT-brain scan and emergency EEG not performed, a treatment was initiated: made of injectable Artesunate (H0-H72), Oritaxim, Amikacin, Ciprofloxacin, a maintenance infusion :( SG5% + electrolytes + Nootropyl + Azantac) and feeding by gavage. The evolution would be marked on D5-D7 by an awakening initiated with Brocas motor aphasia, right hemiparesis, CT scan of the brain, performed: Left frontal hypodensity zone. Under Citicholine(Somazina) and Neuroregulators (Gamalate B6, Surmenalite), resumption of language 24 hours later, with end of tremors (impairment of central gray nuclei) under Artane ½ tablet for 7 days with a good spectacular development. File close and exit authorized with Trausan, Surmenalite and Gamalate B6 for 1 month; an appointment in 1 month with a cerebral CT-scan control.
The second case; she is a 27-year-old patient, admitted for temporo-spatial disorientation and headache. contributory, in whom the clinical examination notes a BP: 158/87 mm Hg, HR: 112bpm, FR: 24 cpm, patient with temporal disorientation spatial, EG altered by suffering mine, Colored eyelid conjunctiva and bulbar anicteric, on normal gynecological examination, on neurological examination; flexible neck and no signs of neuro-meningeal irritation, isocoric and reflective pupils. At the exam paraclinical; GE: Tropho +; incidental blood sugar: 112 mg / dl, Hb: 12 g / l, ESR: 60mm / H, GB: 12200elt, FLN62% L38%, Urinary sed (GB: 5-10 / elt, EC: 5-10 / elt), treatment with Artesunate, promethazine, ceftrin plus. The evolution was marked by a motor aphasia of Broca, a few hours after admission, a cerebral CT scan was urgently requested, not carried out given the financial situation patient, and she was on citicholine (Somazina) as a continuous infusion with antioxidants (VIT C, VIT E) in emergency, neurosedation with phenobarbital. On day 1 of hospitalization, i.e. 24 hours of hospitalization later, we observed the resumption of speech with temporo-spatial orientation, and vital signs in physiological norms. File close and exit authorized with Somazina tablet, Gamalate B6, Overmenalitis for 1 month.
Conclusion
Before any case of acute malarial encephalitis (cerebral malaria), it is of interest to add the neuroregulatory therapeutic regimen; improving the prognosis (rapid recovery), preventing the occurrence of neurological complications often irreversible and reduced morbidity and mortality. And Antimalarials, do not modify the evolutionary process of destruction neuronal and neurological sequelae.
Oral Session 5:
- PEDIATRIC STROKE AND RECOVERY
Title: PEDIATRIC STROKE AND RECOVERY
Biography:
Habiba Abdullahi is a 4th year medical student at Near East University School of Medicine, Cyprus. She is intrested towards the research and developments in Pediatric Neurosurgery.
Abstract:
A stroke occurs when the blood supply to a part of the brain is disrupted or reduced, preventing brain tissue from getting oxygen and nutrients which causes brain cells to die in minutes and according to the part of brain affected, loss of function occurs. In more scientific terms, it is a clinical, radiological, or pathological evidence of ischemia or hemorrhage, involving a defined cerebral vascular territory(1). It is the leading cause of disability in the USA and a major cause of mortality worldwide(2).
Strokes can be categorized as ischemic (inadequate blood supply to the brain) or hemorrhagic (bleeding into the brain); which is the less common type. Although rare, pediatric stroke is the leading cause of morbidity and mortality in children. This is due to delayed diagnosis which is because of delay in seeking medical attention. Stroke, in pediatric patients is defined by the same criteria as adults, however in these patients, unlike adults, the acute presentation is missed. Population-based studies of arterial ischemic stroke(AIS) in children(age 29 days-18 years) estimate an annual incidence of 2.4 per 100,000 persons with a case fatality approaching 4(3),(4). Even amongst the survivors, there are very high chances of long-term disabilities. Over 50% of the survivors have persistent neurologic, cognitive, or psychiatric problems. The management of stroke in pediatric population is also highly challenging due to lack of literature, basing treatment solely on following adult stroke management.
There are different ways of classifying stroke in pediatric patients. By age: from 28 weeks of gestation to 28 postnatal days of life is generally called PERINATAL STROKE which present with focal seizures and sensorimotor deficits as the child ages(5),(6).Some authors have expanded this interval to begin from 20 weeks of gestation because lesions even before the 28th week of gestation has been documented(7). Stroke occurring after 28days of life to 18 years is CHILDHOOD STROKE which presents with acute focal neurological deficits e.g. hemiparesis(5), (6).Perinatal stroke occurs in 1 in 2300 live births while childhood stroke occurs in 2-3 per 100,000(8), (9). Acute perinatal stroke presents shortly after onset with focal seizures and encephalopathy. Presumed perinatal stroke are chronic infarcts, diagnosed in a delayed manner that are presumed to have occurred in the perinatal period(6). These patients exhibit no symptoms in the perinatal period, thus are not detected until a hemiparesis occurs later on within the first year(5). Infants with this present with pathologic early handedness or seizures, which subsequently leads to brain imaging and diagnosis(10).
Ischemic stroke constitutes arterial ischemic stroke (AIS) and venous thrombosis caused by cerebral sinovenous thrombosis(CSVT) and cortical vein thrombosis(6). About 80% of the lesions in perinatal stroke are ischemic(arterial ischemic stroke) and the rest, are due to hemorrhage or cerebral sinovenous thrombosis(CSVT)(11). The ratio of ischemic stroke is significantly higher in newborns, almost 6 times more than in older children(12).
Newborns with AIS typically present with seizures, specifically focal motor seizures involving only one extremity, and this is seen rarely in older children(13)(14). The left cerebral hemisphere is affected in 80% of neonates with unilateral infarctions(14).
In the adult patients, stroke is generally due to atherosclerotic risk factors like hypertension, diabetes mellitus, dyslipidemia, obesity etc. In children and adolescence, atherosclerosis is generally not a causative factor of stroke, but it’s evident that the atherosclerotic process that ultimately causes stroke in adults begins from childhood and that dyslipidemia is more common in children with ischemic stroke than other children(15). Main risk factors in pediatric stroke include both maternal and neonatal factors. It is speculated that normal levels of coagulation factors in mothers and low levels of factors in the infant just before and after the time of delivery contributes to increased stroke risk in neonates(7).Neonates with Acute ischemic stroke sometimes have inherited thrombophilia(16). Other risk factors correlated with neonatal acute ischemic stroke are cardiac lesions, coagulation disorders, infection, trauma and asphyxia(7), (9)(17). Recently, COL4A1 mutations which is a subunit of type IV collagen that plays a role in angiogenesis has been recently linked to intrauterine stroke and porencephaly(18), (19). Some maternal factors, e.g., oligohydramnios, premature rupture of membranes, history of infertility, emergency cesarean section, pre-eclampsia may be associated with perinatal acute ischemic stroke (AIS). Even though all the risk factors mentioned have been proven to increase the chances of AIS, no single cause has been isolated(20), (9).
The most important thing needed for a full recovery in pediatric stroke is adequate management and prevention. The standard of care is certain interventions to obtain physical, occupational, speech and language therapy and neuropsychological interventions(5). Prevention can be done by targeting the risk factors. Therapy, rehabilitation, and recovery is a bit complex in pediatric patients because some deficits are not obvious till a long time after the stroke has occurred. There is little known about the acute treatment and recovery techniques specific to pediatric patients. For management, there is supportive care which constitutes optimization of oxygenation, control of seizures, and the correction of dehydration and anemia(21). Antiplatelet therapy is considered only in neonates with high risk of recurrent AIS due to thrombophilia or congenital heart disease(22), (23). Thrombolysis has been approved for use only in children 18years and older and not considered in neonates, although, there has been recent research that aims to establish the safety and feasibility of thrombolysis using tissue plasminogen activator(tpA) intravenously and intraarterially for AIS in younger children(ages 2-17)(6), (24), . Endovascular procedures e.g. mechanical thrombectomy have been approved for in older children with occlusion but these are not used in neonates because of the small size of their arteries(21), (25).Most of the children with AIS experience residual neurological deficits including cerebral palsy, cognitive speech impairment, and epilepsy(26).
There have been promising therapies to aid in the recovery of pediatric stroke patients. Such therapies include Constraint induced movement therapy (CIMT) to improve motor outcomes. Use of noninvasive brain stimulation to aid in the prognosis or modify outcomes of children after pediatric stroke is beginning to look promising as an adjunctive treatment to promote recovery(5). Stem-cell based treatments have been explored but there is less evidence of its success in pediatric patients(5), (27).
Outcomes after pediatric stroke are good, but moderate to severe neurological impairments are still seen especially between 28 days and 1 year because these are vulnerable ages(28), (29), (30),(31). Another research showed that most of the recovery occurs 2-3 months after stroke, and quality of functional recovery was better in pediatric than the adult population, and it’s believed that the window for recovery is longer for children(32), (33). This could be due to the ‘Kennard principle’ by Margaret A. Kennard which is that younger brains naturally recover better than older brains(34).
Generally, recovery of pediatric stroke depends on age/stage of development, presentation, speed of diagnosis.
Oral Session 6:
- Spine Surgery & Spine Disorders
Title: Medular compression sindrome as a presentation of a spinal epidural lynphoma.
Biography:
Graduated as a Doctor of Medicine from the University of Medical Sciences of Matanzas in July 2016. In September of that same year, I began my residency in the specialty of Neurosurgery at the Faustino Perez University Hospital in Matanzas, Cuba. After 2 years of work as a resident doctor at that hospital, I was accepted as a resident doctor of neurosurgery at the Institute of Neurology and Neurosurgery of Cuba, where I graduated as a General Neurosurgeon on January 28, 2021. Now I work as a General Neurosurgeon at the Matanzas province treating adults and children with neurosurgical pathologies.
Abstract:
Introduction: Lymphomas are solid tumours of the immune system. Spinal cord compression by this tumors is a late manefestation and not always present in all of patients. Sometimes, lynphomas can be present only in the spinal epidural space but this is a very reare condition.
Case report: This is a 23 years old patient who 6 month ago started with dorsal pain after a sudden movement. With time, the pain got worse in intensity and frecuency. Four month after his first manifestation noted a progressive loss of weight and weaknes in both lower limbs.
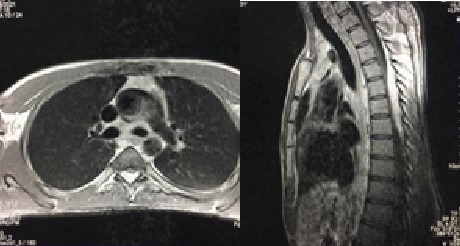
Discussion: In the CT and MRI studies, we found images suggestive of lymphadenopathy in the mediastinum and abdominal cavity, as well as in the dorsal spine an intra-spinal extradural image that enhancement with contrast. Thinking in a paraparesis caused by a extradural lynphoma, the patient was taken to the operating room and a three- space laminectomy was performed with a gross total ressection of the tumor. Histopathological examination revealed a Hodgkin lynphoma and 5 days after surgery the patient presented improvement in the muscular strength of the lower limbs. He was transferred to the oncology service to begin with adjuvant chemotherapy and radiotherapy treatment.
Conclussion: Despite the low incidence of lymphomas with spinal epidural presentation, it is a diagnosis to bear in mind when differentiating intra-spinal extradural tumors. Surgery in patients with signs of medullary compression that are clinically expressed with progressive neurological deterioration should be performed as soon as possible to achieve an adequate improvement of the neurological picture.
Title: WORKING WITH LIMITED RESOURCES IN ARMED CONFLIECT COUNTRY FOR TRANSPORTATION & PREHOSPITAL MANAGEMENT OF TRAUMATIC CERVICAL SPINAL CORD INJURIED PATEITNS, 89 CASES
Biography:
Dr.Hamed Shir Shinwari is consultant neurosurgeon in Daudzai Medical Complex, Nangarhar Afghanistan. He graduated from Nangarhar Medical Faculty (NMF) in 2014 and joined neurosurgery training in 2016 and graduated from Jamhuriat tertiary hospital in 2020, he operated more then 800 neurosurgery cases. He is the first Afghan neurosurgeon who represented Afghanistan in WFNS. He also written 11 medical books 4 of which is related to neurosurgery. He was the first author of Pashto neurosurgery book in Pashto language.
Abstract:
Abstract
Introduction:
Traumatic cervical spinal injury (SCI) is one of the most devastating conditions with high rates of morbidity and mortality. First aid, transportation and on time management of such disorder play a vital role for favorable outcome and prognosis.
The aim of this study to review the prehospital, immobilization, transportation and management of traumatic cervical spinal injury and its outcome.
Materials & Methods:
The department of Neurosurgery of Jamhuryte Hospital, Kabul Afghanistan, carried out this one year prospective case series from March 2017 to Mach 2018 to evaluate the pre-hospital management of SCI and its outcome.
Results:
Eighty-nine cases were reported over period of one year. The SCI cases were more common among male (78.6%) compare to female gender. The main age group were 20 to 45 year of age which were affected (73.8%). The main causes of morbidity and mortality were high amongst those who were involved in motor vehicle accident (45.8%) fall from height (41.9%). Twenty percent (20%) of patients transported from the accident scene to hospital who has had cervical collar stabilization. An average patient’s admission time to the emergency department of hospital was 16-72 hours past-accident, accounted for 22.9%. The most popular mode of transportation from the scene to the hospital was Private cars (59.2%).
Associated injuries with SCI among these patients were long bone fractures (6.8%), traumatic brain injury (45.8%), and abdominal trauma (1.9%). Among cervical injury the sub-axial injury at the level of C3/C7 (76.7%) were the commonest.
During admission, the complete and incomplete spinal cord injuries rates were 43.1% and 64.9% of patients, respectively.
Surgical procedures for SCI management performed in (25%) of the patients. With favorable outcome, who had regained motor and sensory recovery with no post-operative complications.

Figure 1 shows patient with cervical injury and traction is done with very limited resource in radiology department. Stone are used for traction.
Conclusion:
In Afghanistan traumatic cervical spinal cord injury is still one of the most catastrophic conditions with high rates of morbidity and mortality safe and rapid transportation of the cervical spinal cord injured patients to the medical facilities for definitive care has been a fundamental concept to improve the treatment outcome and to reduce the complications as whole.
Title: Clinical Outcome of Percutaneous Laser Disc Decompression in Patients with Lumbar Disc Herniation: A Pilot Study in a Low-Resource Facility
Biography:
Dr. Sajjad Saghebdoust is a medical doctor who graduated from Mashhad University of Medical Sciences, Iran. He has a postgraduate degree in healthcare MBA and he is currently an MPH candidate at Shiraz University of Medical Sciences, Iran. He was awarded a position as a neurosurgery research assistant at Razavi Hospital, Mashhad, Iran and he is a member of Iran’s National Elite Foundation. Since his graduation from medical school, Dr. Saghebdoust has been involved in different studies in endovascular neurosurgery, spine surgery and functional neurosurgery.
Abstract:
Abstract:
Statement of the Problem: Herniation is broadly defined as a localized or focal displacement of disc material beyond the limits of the intervertebral disc space. The disc material may be nucleus, cartilage, fragmented apophyseal bone, annular tissue, or any combination thereof. Laser surgery is one of the treatment modalities for treating patients with lumbar disc herniation. This study aims to examine the effect of laser disc decompression in patients with lumbar disc herniation. Methodology & Theoretical Orientation: This study was conducted on 58 patients who underwent Percutaneous Laser Disc Decompression (PLDD) (optical fiber inserted through an 18G needle, 8 joules, and 8 watts). Eligible patients were treated with PLDD according to the treatment protocol. They were monitored before and after treatment using the comparing Verbal Analog Scale (no pain, mild pain, moderate pain, severe pain), the Visual Analog Scale (VAS) Pain Score (0 (no pain) to 10 (most pain)) before and after the surgery, and by completing a questionnaire. In all statistical tests, p values under 0.05 were considered significant. Findings: The mean age of participants was 63.19 ± 13.48 years. Regarding gender, 34 patients (58.6%) were male, and 24 patients (41.4%) were female. mean VAS score before surgery was 8.73 ± 1.29 and mean VAS score after surgery was 5.22 ± 2.71, and the pain was significantly reduced (P<0.001). Conclusion & Significance: According to the post-PLDD pain reduction in our population, PLDD can be considered an appropriate method for treating lumbar disc herniation in carefully selected patients.
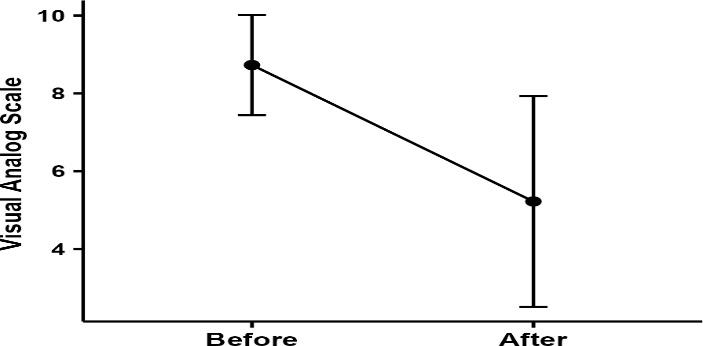
Figure1: Patients’ pain scores before and after the intervention
Recent Publications (minimum 5)
- Momenzadeh S, Koosha A, Kazempoor Monfared M, et al. The Effect of Percutaneous Laser Disc Decompression on Reducing Pain and Disability in Patients With Lumbar Disc Herniation. J Lasers Med Sci. 2019;10(1): 29-32. eng.
- Brouwer PA, Brand R, van den Akker-van Marle ME, et al. Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: Two-year results of a randomised controlled trial. Interv Neuroradiol. 2017;23(3): 313-24. eng.
- Erbas Y, Pusat S, Erdogan E. Percutaneous Laser Disc Decompression: Retrospective Analysis of 197 Cases and Review of The Literature. Turk Neurosurg. 2015;25.
- Rahimzadeh P, Imani F, Ghahremani M, et al. Comparison of percutaneous intradiscal ozone injection with laser disc decompression in discogenic low back pain. J Pain Res. 2018;11: 1405-10. eng.
- Kasch R, Mensel B, Schmidt F, et al. Disc volume reduction with percutaneous nucleoplasty in an animal model. PLoS One. 2012;7(11): e50211.








